And yet they rise
By Kinya Kaunjuga
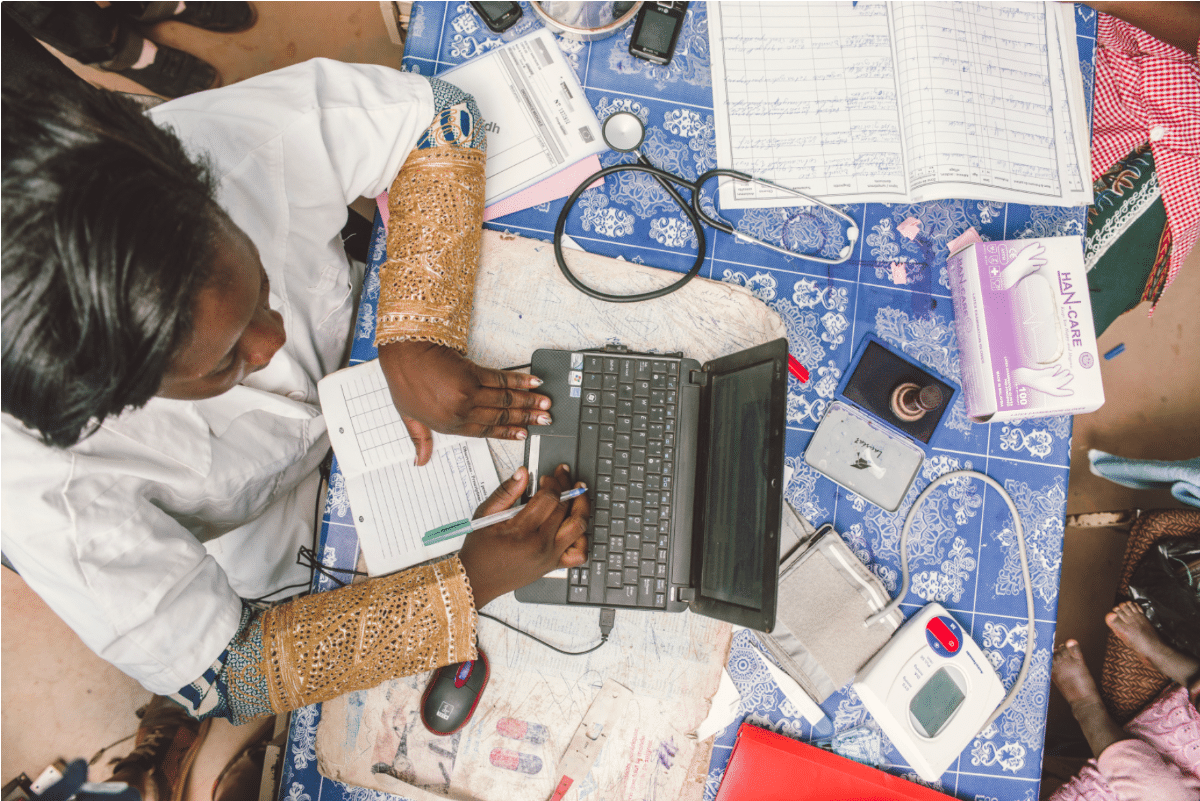
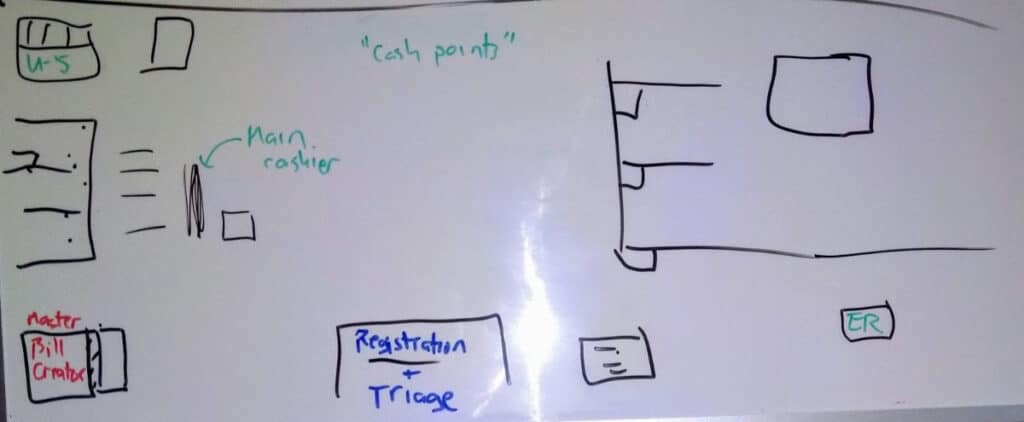
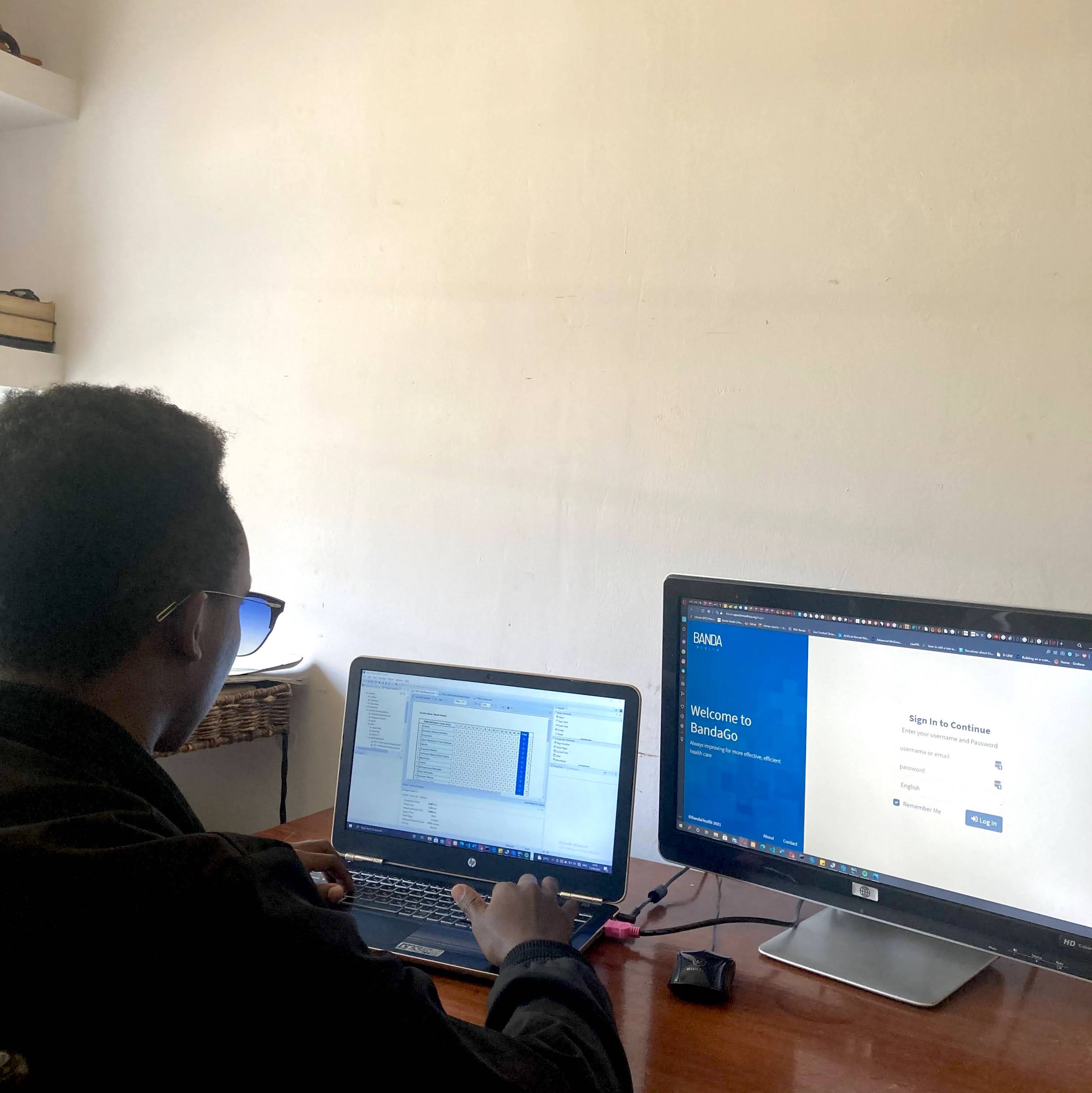
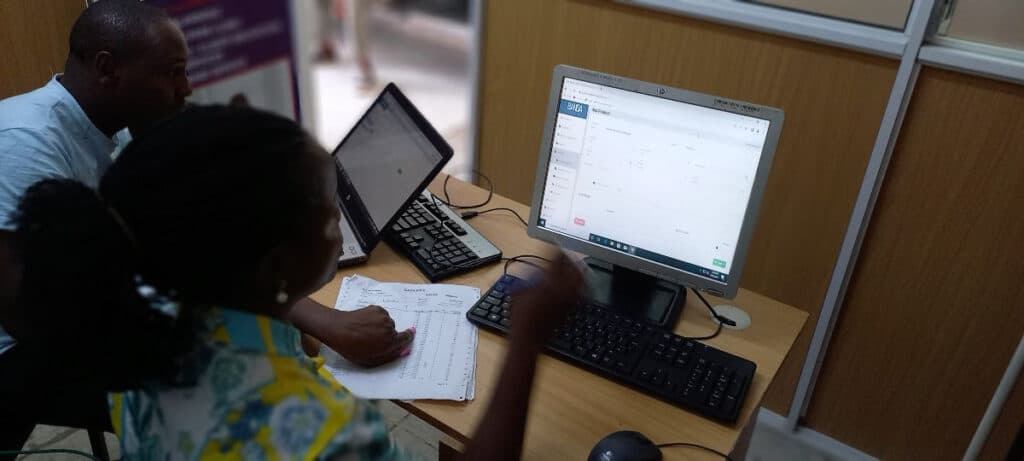
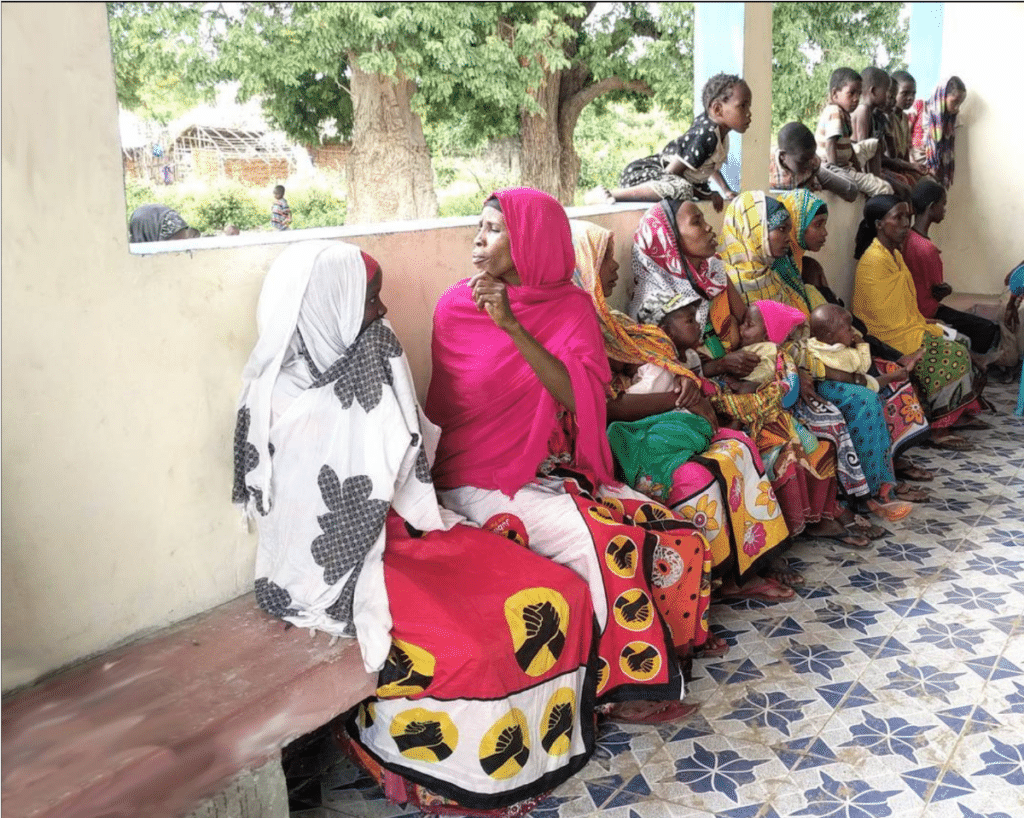
In our work, there are medical clinics that consistently blow us away with their determination to hone their skills at using BandaGo.
As technology innovators, we call them “super-users” because of their drive to apply every benefit of technology to impact their patients.

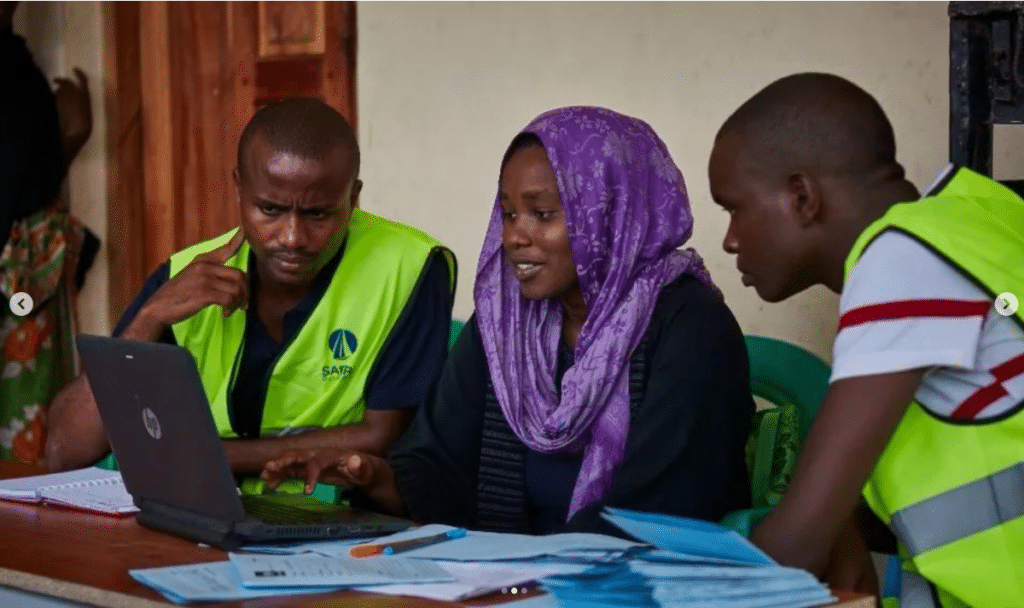
From her poised demeanor and quick keystrokes on a shiny purple laptop, one would never guess that Silpa has battled cerebral palsy since childhood. She explains that her aunt Sylvia, the Christian nurse who co-founded the Matangwe Community Health & Development Program (MCHDP), was part of her family “win-team” to aggressively get the disease treated and managed. She says she is lucky that her mother got her diagnosed early in her childhood unlike many parents in developing countries who discover their children have cerebral palsy too late for physical therapy to impact their limbs.
Her family’s care and attention ensured that she never missed a beat in her growth and education. She had attended schools with playgrounds she could never run around on. But as I witnessed her interact with Mike during her training, it is clear her brain is where she runs.
Her well versed knowledge of the system, Matangwe’s processes, and her ideas to apply accounting best practices using BandaGo, made me aware that her weak limbs are just annexes to her ingenuity.
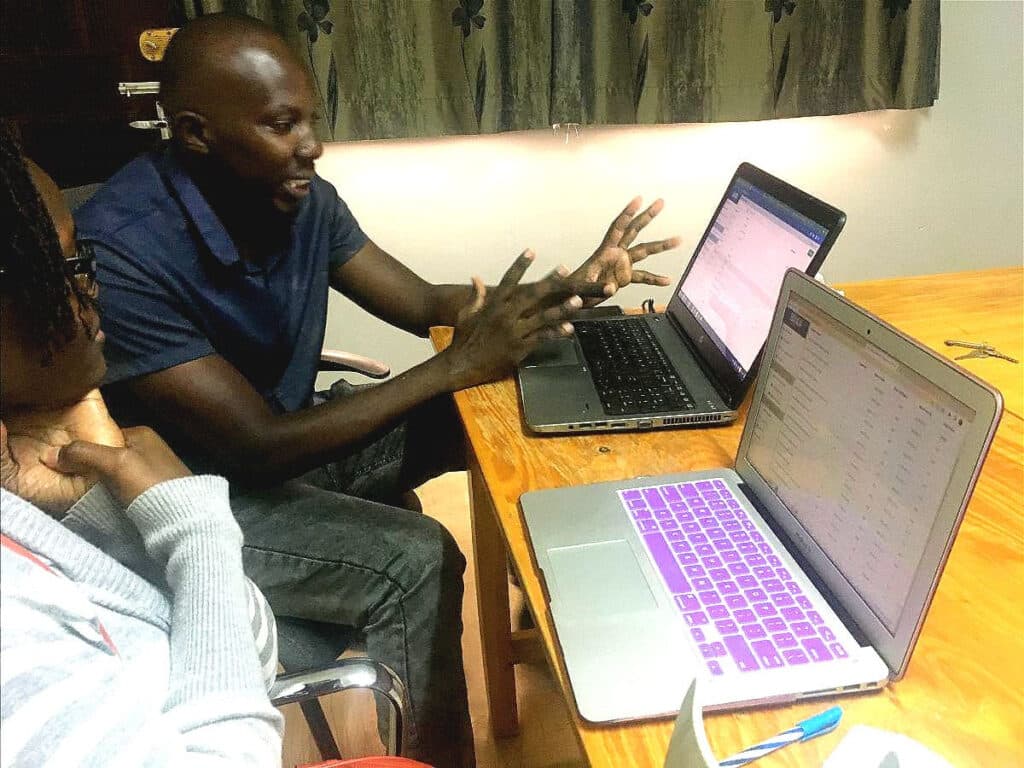
As she prepared to leave the Banda Health office when her training was complete, Mike offered to carry her backpack and she responded, “It’s not that heavy.”
We watched her maneuver one of her arms into a crutch, drag her paralyzed legs to face the door, and twist her waist which guided her shoulders to turn. Then she arose, steadied the shaking and veering of her body and started to move.
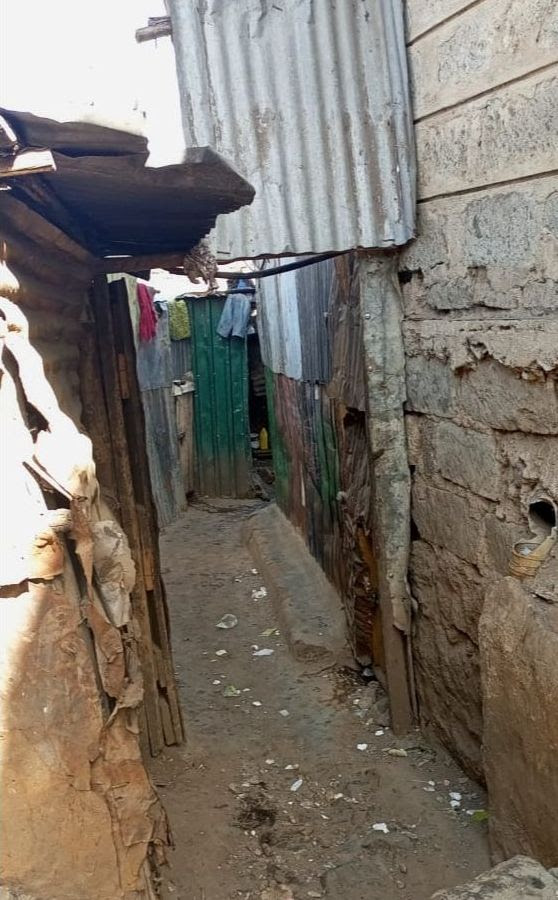
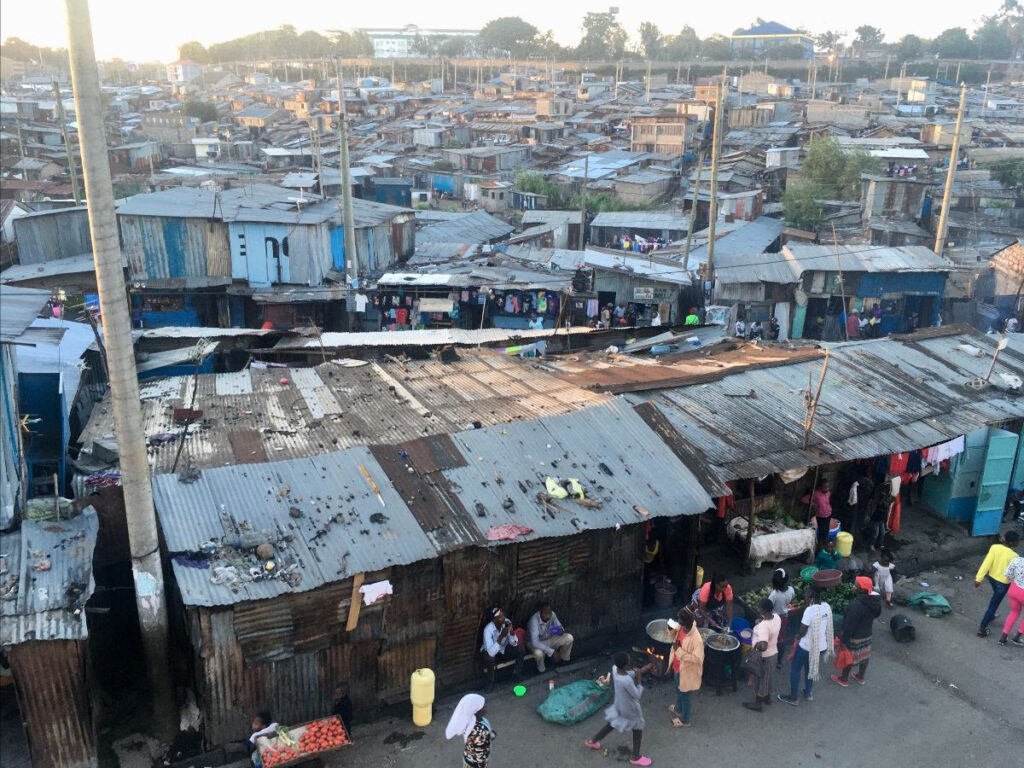
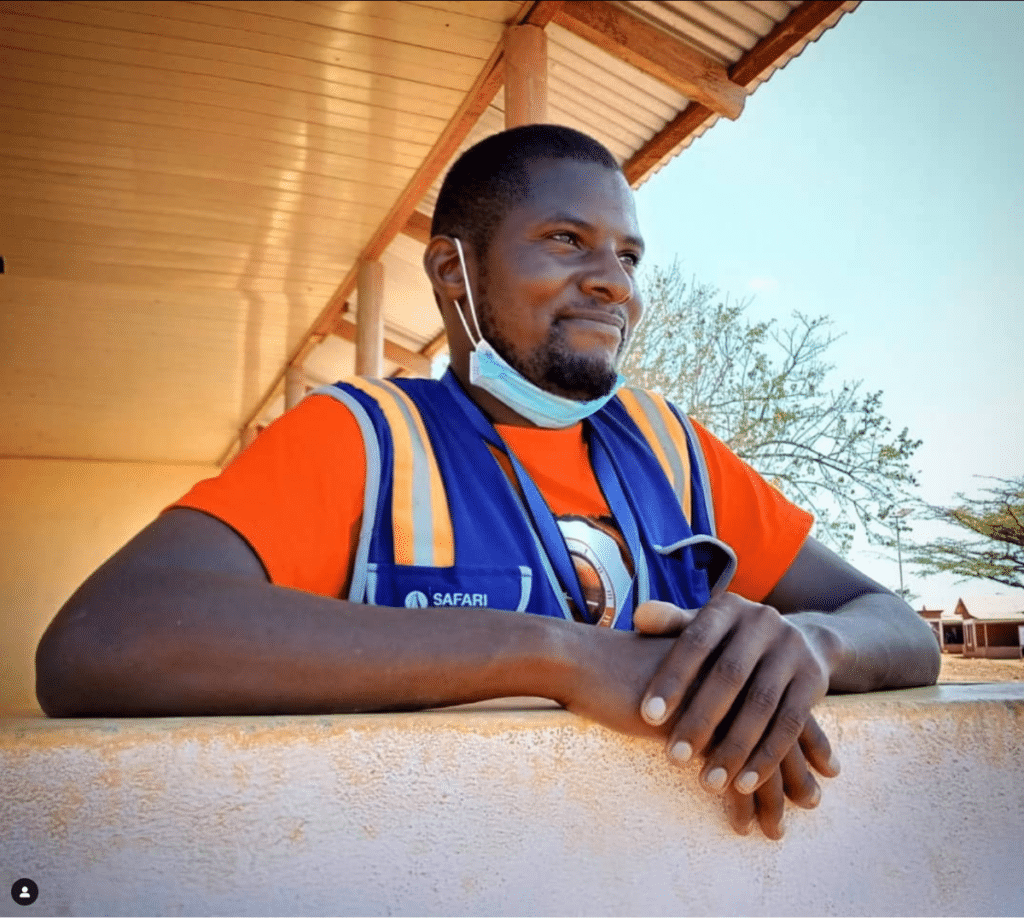
Instinctively, Mike grabbed her bag and she smiled. What had transpired was more than system training. As Banda Health our adventures revolve around supporting those who own and run poor clinics treating even poorer patients. They are our heroes because they endure their own personal hardships and yet they rise to help many get good healthcare.
Maybe like Silpa, they face each arduous activity treating patients in slums and remote villages with the mantra, “its.not.that.heavy.”
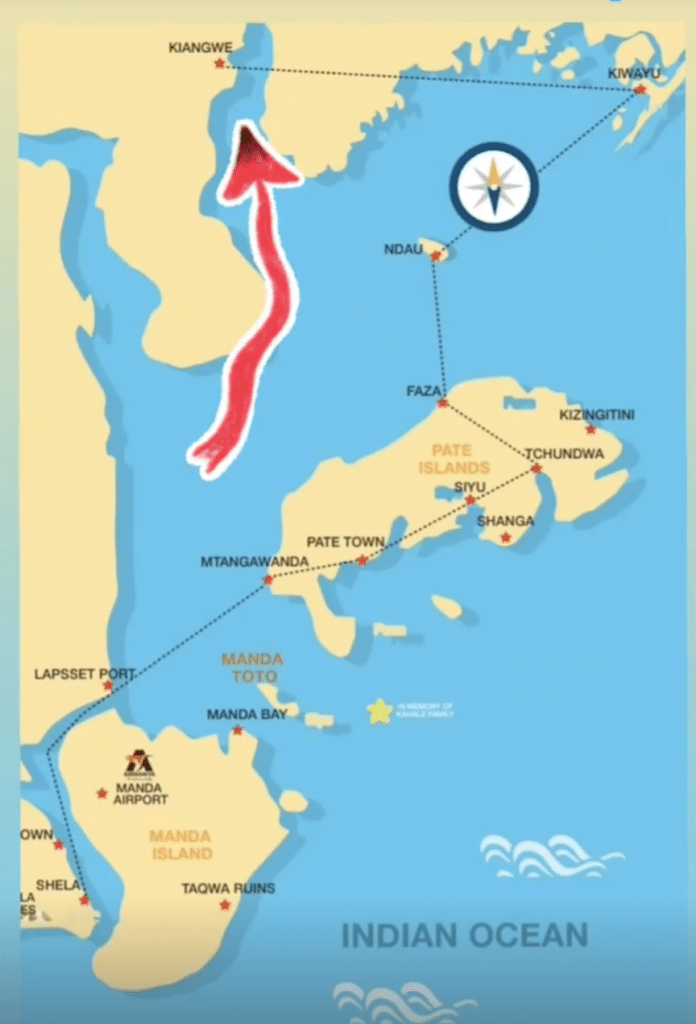
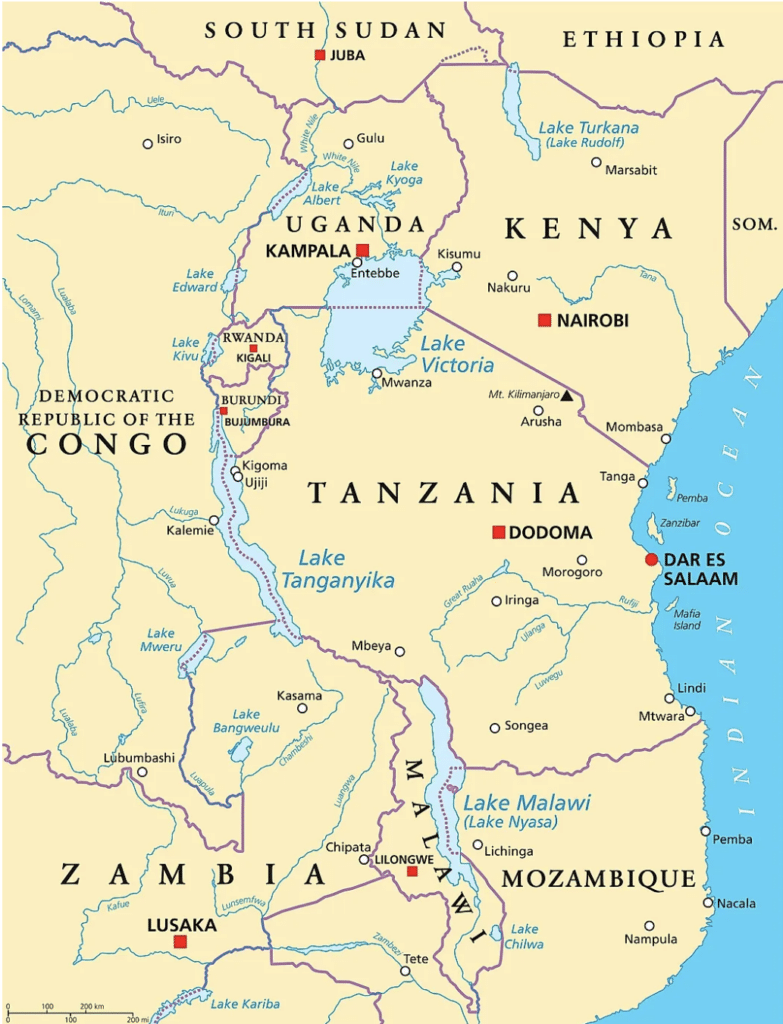
For the history buffs: Here are Africa's Great Lakes. Can you trace the source of the Nile?
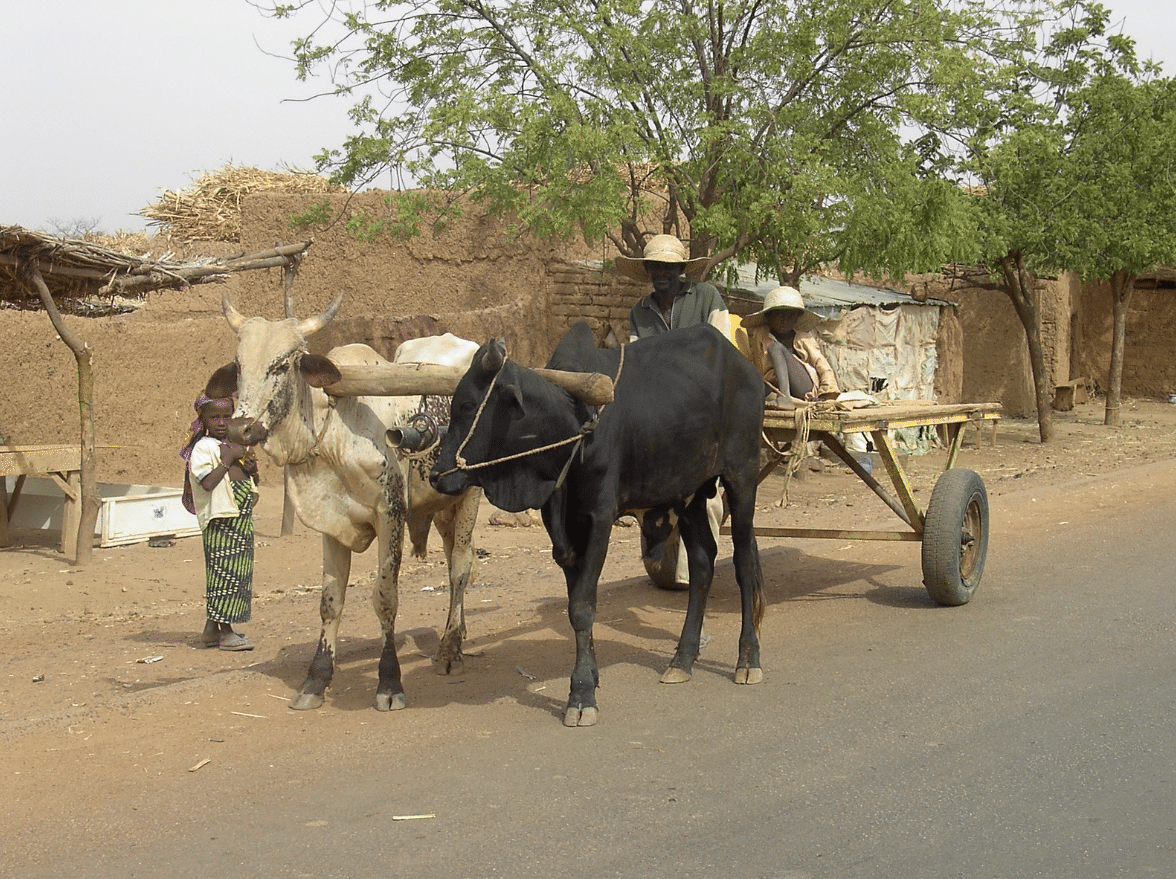
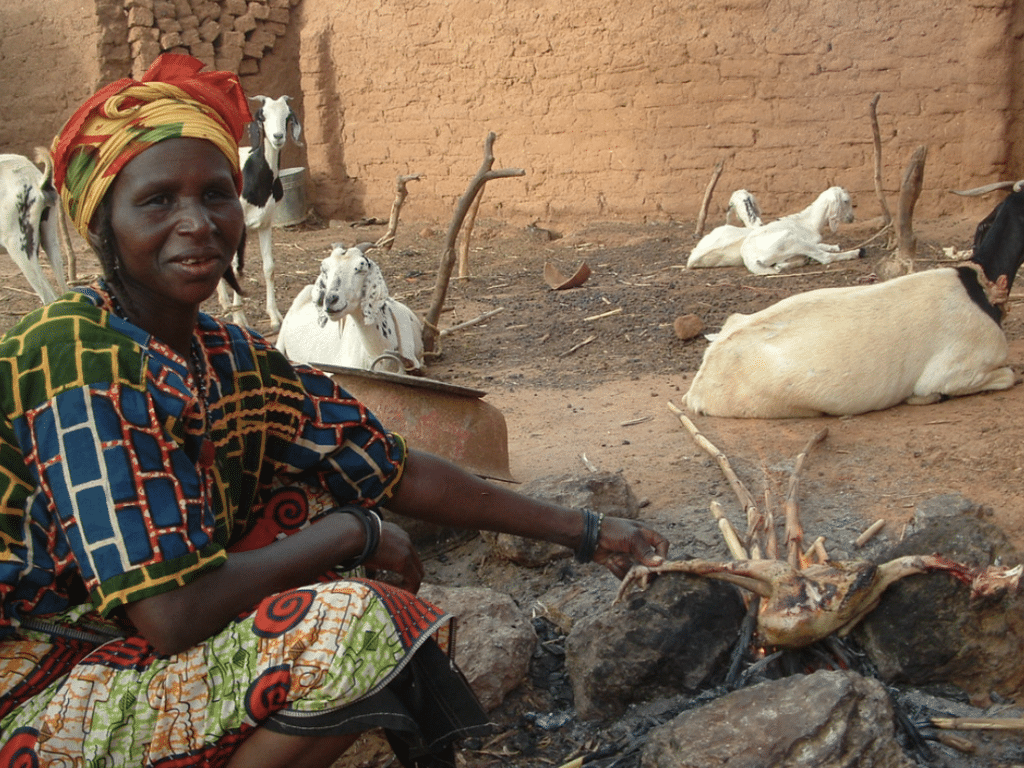
From the Sahara to the Savannah, thank you for joining us on our "Adventures with Banda" as we help medics tackle the barriers to accessing good healthcare for the poor.
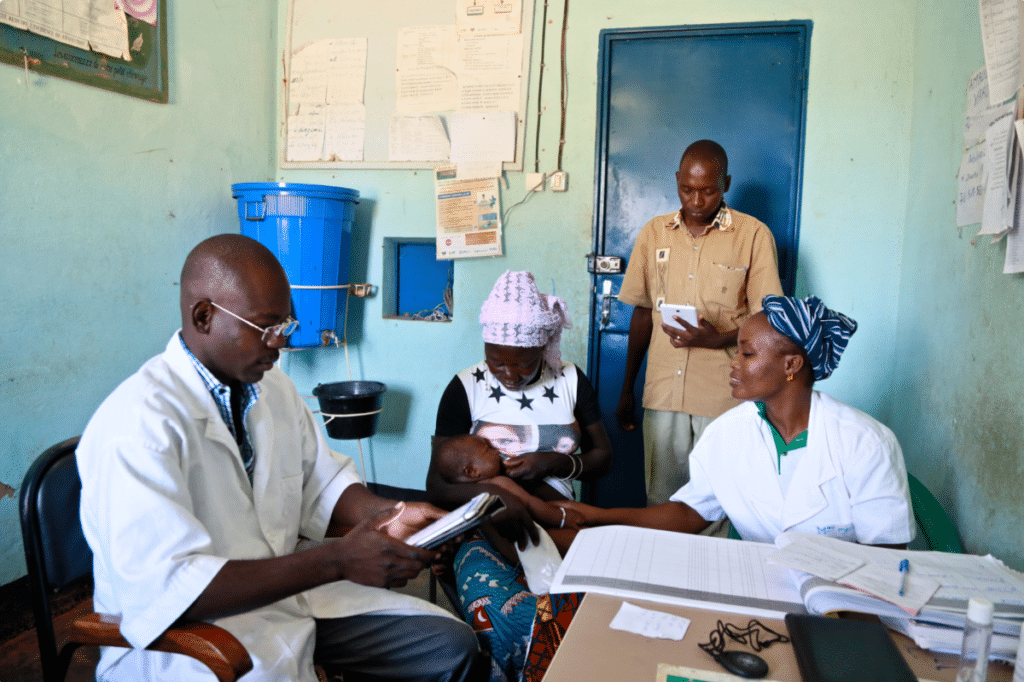
$5000 helps us improve BandaGo and get it in another clinic
Our work wouldn’t be possible without your support. Thanks to you, there are now over 80 frontline medical clinics using BandaGo in 3 countries across Africa.
Photos courtesy: ©Banda Health, ©Tdh/Ollivier Girard.

Kinya Kaunjuga
Kinya brings passion, an infectious laugh and 15 years of experience in the corporate and non-profit world to Banda Health. A Texas A&M alumni with a degree in Journalism and Economics, she says, "I love doing things that matter!"